Abstract
Introduction: Asthma occurs in up to 28% of patients with sickle cell disease (SCD) and is associated with increased incidence of vaso-occlusive pain, acute chest syndrome (ACS), and mortality. Systemic steroids are the standard treatment for acute asthma and are often used in patients with SCD, especially as clinical symptoms of acute asthma exacerbations may often overlap with those of ACS. The risk of rebound pain following treatment with corticosteroids has been reported in other studies. However, the temporal association and the factors associated with the risk of rebound vaso-occlusive pain, specifically in those with co-morbid asthma diagnosis, have not been well described.
Objective: To evaluate the temporal association between the use of systemic corticosteroids in patients with SCD and asthma and the factors associated with the risk of rebound vaso-occlusive pain.
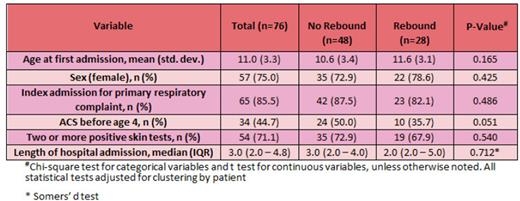
Methods: Patients with confirmed SCD and asthma, between ages 4-18 years of age, and admitted between 2006 and 2009, were eligible. Based on their associations with SCD and asthma, the co-variables of interest evaluated included hydroxyurea (HU) usage, age, sex, atopy, indication for hospitalization, and length of hospital admission. Participants were included if they received systemic glucocorticoids (dexamethasone, methylprednisolone, prednisone, prednisolone) during admission. Participants were excluded if they were receiving chronic blood transfusion therapies or participating in clinical trials involving blood transfusions. Our primary end-point was readmission for rebound vaso-occlusive pain within 14 days of the index admission. Continuous variables were analyzed with the mean (std. deviation) or median (inter-quartile range), based on the distribution, and compared by group with a t test or Somers'd statistic. Categorical variables were analyzed with counts (percent) and compared with a Chi-square statistic. All tests were adjusted for clustering by patients.
Results: Fifteen distinct patients, 9 (60%) females, with a total of seventy-six admissions with administration of corticosteroids were included in the analysis (Table). Fifty-seven (75%) of admissions occurred in female patients with a median length of hospitalization of 3.0 days (IQR 2.0 - 4.8). Of the 76 episodes of corticosteroid use, 65 (85.5%) were due to a primary respiratory illness. There were twenty-eight (36.8%) readmissions for rebound vaso-occlusive pain with a median time to readmission of 3.0 (IQR 2.0 - 6.0) days. Amongst all patients, neither sex, history of atopy (>=2 positive skin sensitization tests), indication for hospitalization, or length of hospitalization were associated with the risk of readmission for rebound pain (p=0.425, p=0.540, p=0.721 respectively). Only 2 patients with 5 admissions were documented to be on HU and so we could not assess the relationship to rebound with HU usage. There was a trend for an association of history of early ACS and risk of rebound vaso-occlusive pain. Patients with ACS before the age of 4 were less likely to experience rebound vaso-occlusive pain compared to those without early ACS (P=0.051).
Discussion: Our data shows that patients with sickle cell disease and asthma treated with corticosteroids are at risk for readmission due to rebound vaso-occlusive pain in more than one third of episodes (36.8%) following initial corticosteroid exposure. Our study did not identify any specific factors associated with risk of readmission for rebound pain following corticosteroid use. While corticosteroids are life-saving in status asthmaticus, the risk for rebound pain is significant and clinicians should work to optimize chronic asthma therapy to prevent the need for systemic corticosteroids in asthma exacerbations in patients with SCD.
Disclosures
DeBaun:Novartis, GBT, Vertex, and Forma Pharmaceutical: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal